This tutorial covers the forces controlling fluid balance between the blood and the intercellular fluid in the tissues.
You can navigate through this tutorial using the buttons at the top of the screen.
The tutorial will ask you questions. Click on your chosen answer to see feedback; click the answer again to make the feedback disappear. When you're finished with one page, click the navigation button for the next page to move ahead.
Have fun! Click on button '1' to see the first page of the tutorial.
Page 1
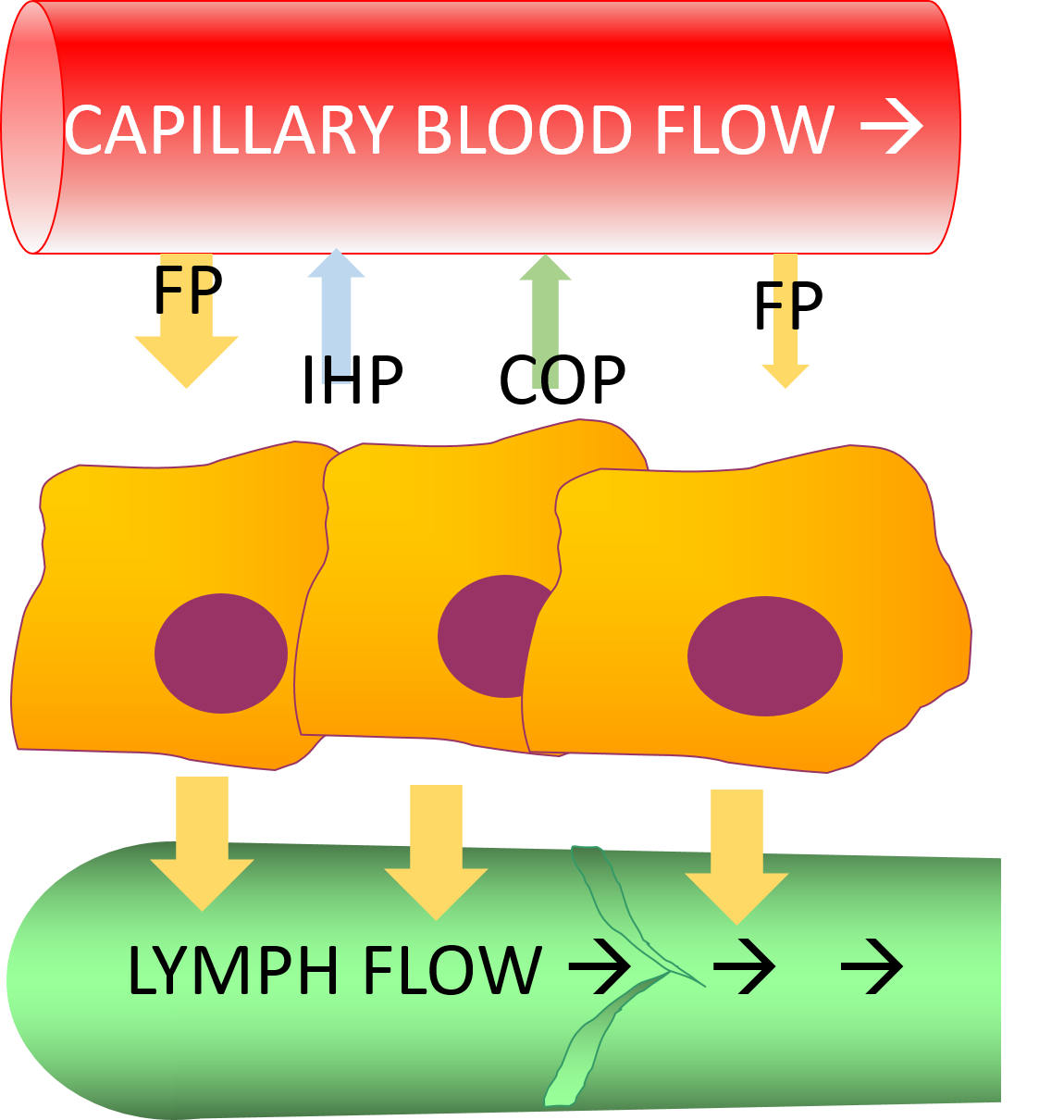
As blood passes through your capillaries, some of it leaks out across their walls into the interstitial fluid, the space between the cells. Forces pushing fluid out of the capillaries include blood pressure and gravity.
FP = filtration pressure
The sum of these forces is called the filtration pressure. It is greatest at the arterial end of the capillary, where the blood pressure is highest, and less at the venous end, where blood pressure is lowest. Because of gravity pulling the blood downward, the filtration pressure is higher in the capillaries in dependent parts of your body. That's why edema often occurs in the ankles and feet.
Page 2
Because your tissues are surrounded by membranes that don't stretch, they can't just expand as they gain fluid. The fluid will build up in the tissues and push back against the capillary wall, opposing the filtration pressure.
FP = filtration pressure
IHP = interstitial hydrostatic pressure
This is called the interstitial hydrostatic pressure.
Page 3
The plasma contains more proteins than the interstitial fluids do, so osmosis causes some tissue fluid to move into the capillaries.
FP = filtration pressure
IHP = interstitial hydrostatic pressure
COP = capillary colloidal osmotic pressure
This is called the capillary colloidal osmotic pressure. 'Colloidal' means it is caused by proteins, rather than other solutes.
Page 4
The filtration pressure is usually larger than the opposing forces, so a larger volume of fluid enters the tissues than is removed from them. The lymph vessels remove this excess fluid.
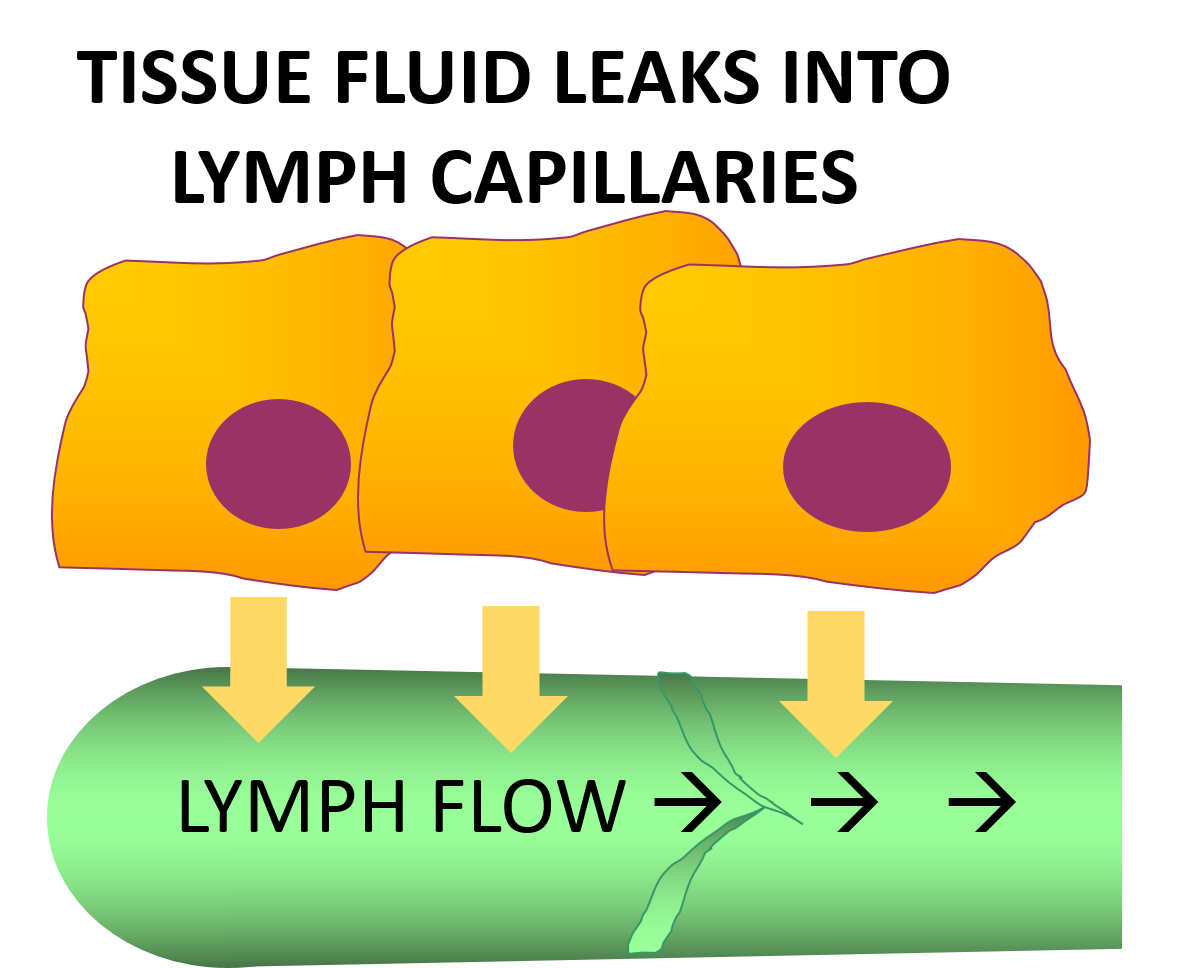
Fluid diffuses into the lymph vessels, and then when the tissue moves the fluid is squeezed past valves, which will not allow it to return to the tissues. The lymphatic fluid flows up to the lymph nodes, where white blood cells remove pathogens from it, and then is emptied back into the venous blood returning to the heart.
As a result, a constant flow of fresh fluid passes over the tissues - from the capillaries, over the cells, and to the lymph vessels.
Page 5
When you understand this process, you should be able to predict how different situations will affect fluid tissue levels.
FP = filtration pressure
IHP = interstitial hydrostatic pressure
COP = capillary colloidal osmotic pressure
Interstitial hydrostatic pressure
Capillary colloidal osmotic pressure
Raising his feet made Mr. K's swelling go down, but he has to go to work tomorrow. The nurse recommended he wear pressure stockings. How will these help reduce his swelling?
By decreasing filtration pressure
By increasing the interstitial hydrostatic pressure
By decreasing capillary colloidal osmotic pressure
Mr. K's doctor is looking into the cause of his swollen feet, and she's found some signs of liver failure. The liver is responsible for making plasma proteins. How coud liver failure have caused Mr. K's edema?
By increasing filtration pressure
Page 6
Here's a page ESPECIALLY FOR PATHO STUDENTS. Let's relate pathophysiology concepts and disease states to edema formation. Try to explain each of the cases; then click on the case to see the answer.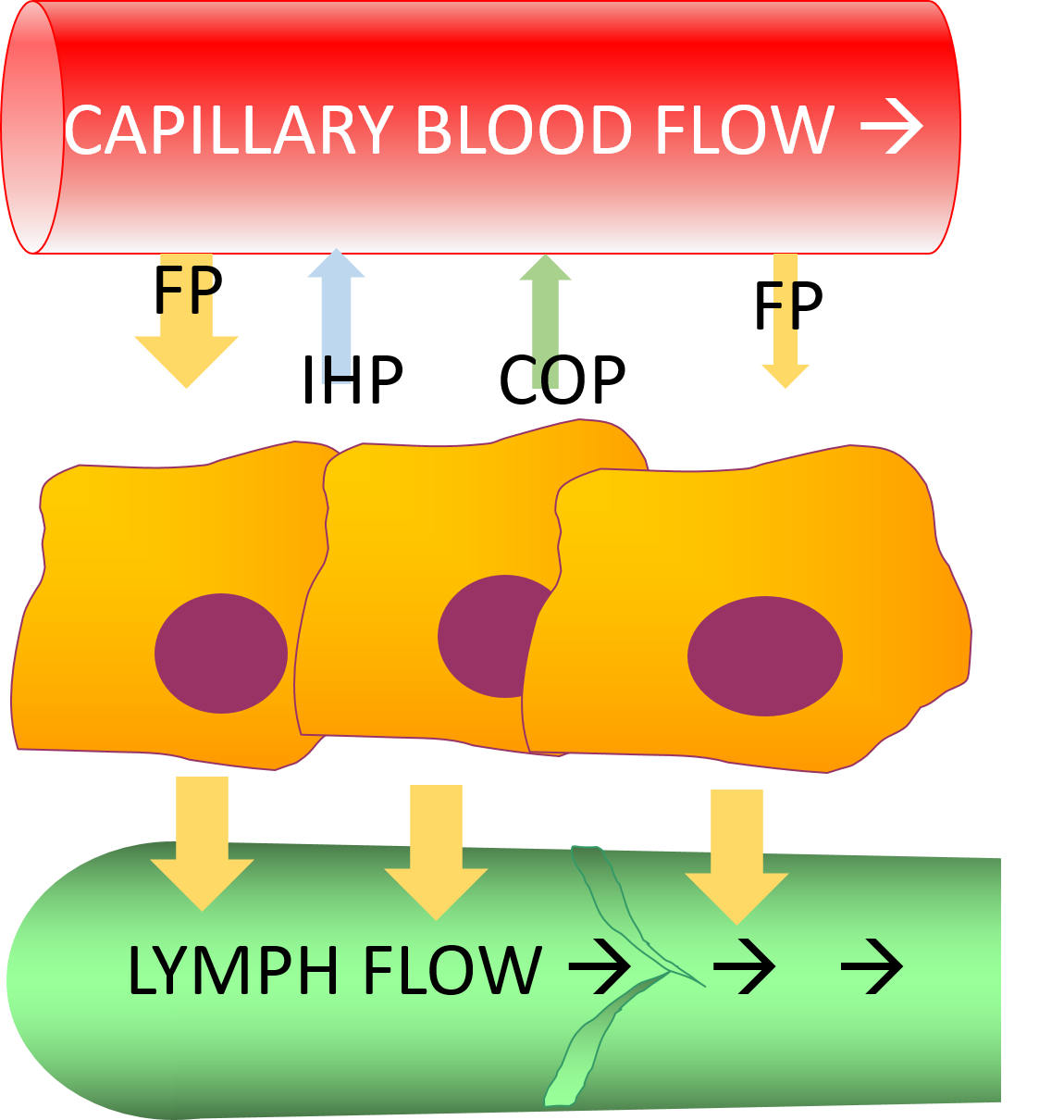
FP = filtration pressure
IHP = interstitial hydrostatic pressure
COP = capillary colloidal osmotic pressure
Page 7
As edema develops, more and more fluid accumulates in the intercellular spaces. These spaces contain a protein-rich tissue gel, which absorbs the water. This holds the water in position.
When the tissue contains more water than the tissue gel can absorb, the excess water is not held in position and can move about in the tissue. This causes pitting edema; pressing a finger into the tissue will displace the water, leaving a dent.
In normal and pitting edema, the fluid filtering out of the blood into the intercellular fluid contains solutes as well as fluid. Usually, intercellular fluid and the cells are in osmotic balance, so that even when the tissue is edematous, the cells don't swell or shrink much. If the blood is hypotonic, though (as in somene who has drunk too much water), the filtrate out into the intercellular fluid will also be hypotonic. What will happen to the cells then?
This is the end of the short review of lymph and edema!
Material in this tutorial is drawn from Porth, C.M. (2014) Essentials of Pathophysiology, 4th Ed.