This tutorial will take you through a basic introduction to kidney structure and function.
You can navigate through this tutorial using the buttons at the top of the screen.
The tutorial will ask you questions. Click on your chosen answer to see feedback; click the answer again to make the feedback disappear. When you're finished with one page, click the navigation button for the next page to move ahead.
Have fun! Click on button '1' to see the first page of the tutorial.
Page 1
Waste Removal
Animals need kidneys to get rid of wastes that are produced by their cells. The major category of wastes we're concerned with are nitrogenous wastes; these are made when your cells break down amino acids for energy.
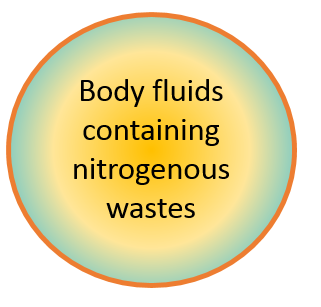
In this cross-section of a simple animal, nitrogenous wastes are being released into the body fluid. They will quickly poison the creature if they can't be removed!
The simplest solution would be to just have a pore in the side of the animal, letting the wastes leak out. I bet you can predict the problem with this, though!
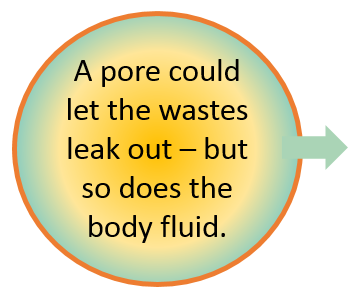
How can our animal keep the good stuff while letting the bad stuff leak out? The answer is to pass the fluid through a tubule made of cells. The cells can sort out the stuff in the tubule, deciding what to save and what to excrete.
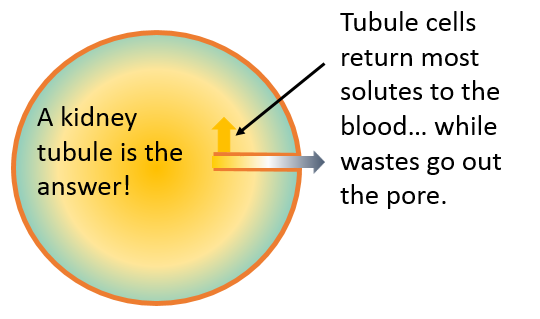
This is the basic kidney! It's just a tube of cells that sorts what you need to keep from what you need to get rid of. The tube is called a nephron.
Of course, large animals like you and me need more elaborate kidneys.
Page 2
To start out with, you and I have cells in our body fluid - red blood cells, white blood cells, things we don't want to lose in our urine. We also have a lot of important proteins in our blood. So we need a filter on the inside end of our nephron, to keep those things from leaking into the urine.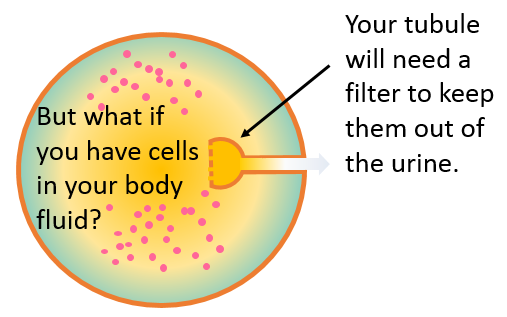
Even more troublesome, though: we don't just let our body fluid slosh around inside us. We put most of it in blood vessels. So that nephron filter has to butt right up against a bunch of blood vessels.
This is the basics of your kidney! Here are the three major processes that form urine:
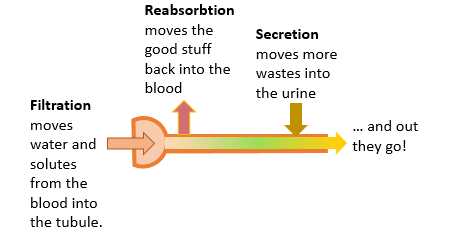
Filtration is when body fluids leak into the nephron through the filter.
Reabsorbtion is when cells of the nephron move compounds back into the blood. The cells reabsorb things like glucose, amino acids, and Na+. Water is reabsorbed too, because it follows these solutes by osmosis.
Secretion is when cells of the nephron move things from the blood into the urine. A good example of secretion is when the Na+/K+ ATPase turns on and moves K+ into the urine.
Page 3
Filtration
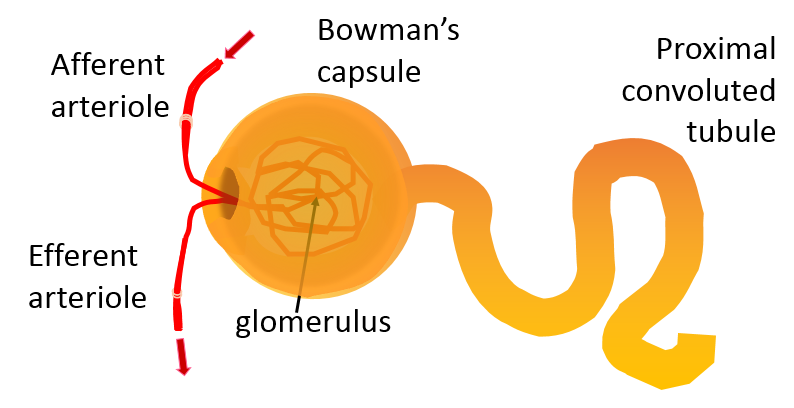
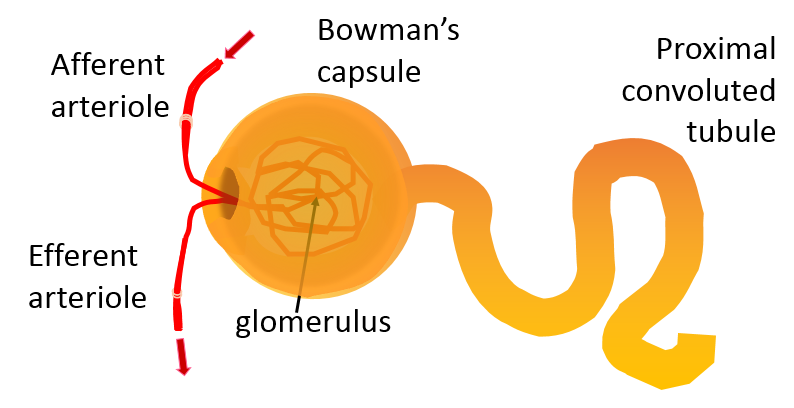
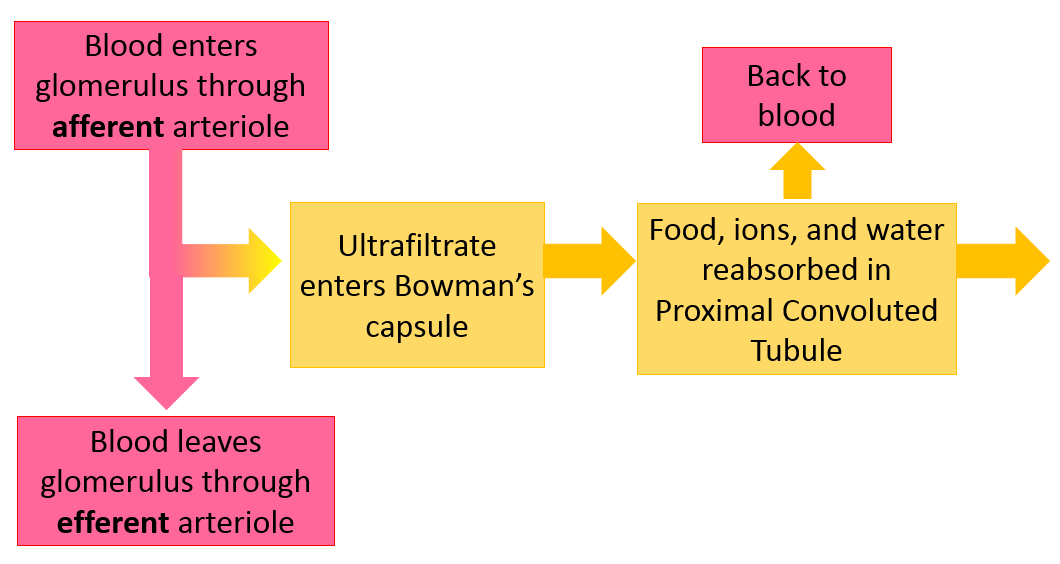
First, let's get some terminology out of the way. Your blood passes into a 'ball' of capillaries called the glomerulus (pronounce it as if it glows).
The end of the nephron wraps around this ball of capillaries. This expanded end of the nephron is called Bowman's capsule.
 An unsavory analogy: It's like when you put your hand in a plastic bag to pick up after your dog. The dog poop would be the glomerulus, and the plastic bag would be the walls of the nephron tube and Bowman's capsule. Lucky for you, the plastic bag doesn't let anything filter through!
An unsavory analogy: It's like when you put your hand in a plastic bag to pick up after your dog. The dog poop would be the glomerulus, and the plastic bag would be the walls of the nephron tube and Bowman's capsule. Lucky for you, the plastic bag doesn't let anything filter through!Image modified from Pixabay, used under a Creative Commons license
The fluid that goes through the filter into your kidney tubule is called ultrafiltrate. It's actually pretty nice stuff, full of water, ions, and food.
To keep your blood clean, you need to filter about 115-125 mL of it every minute. That's called your glomerular filtration rate, or GFR. To manage this, you need lots of nephrons - from 200,000 to over 2.5 million in each kidney! 1
1 - Bertram, J. F., Douglas-Denton, R. N., Diouf, B., Hughson, M. D., & Hoy, W. E. (2011). Human nephron number: implications for health and disease. Pediatric Nephrology (Berlin, Germany), 26(9), 1529–1533. https://doi.org/10.1007/s00467-011-1843-8
Page 4
Before we move away from the filter, take another look at the blood vessels bringing blood into the glomerulus and taking it away again. Do you spot anything unusual about these vessels?
No, small vessels bringing blood to capillary beds are always called arteriolesNo, small vessels bringing blood to capillary beds and taking it away again are always called arterioles
Yes, small vessels bringing blood to capillary beds are always arterioles but vessels taking it away again should be called venules.
What do arterioles have that no other vessel has?
oxygenated blood
valves
sphincters
What do you think these structures are used for?
keeping O2 delivery constant
regulating GFR
regulating blood pressure
What system would constrict the sphincters in the afferent arteriole?
the voluntary motor system
the parasympathetic system
the sympathetic system
Which sphincters would you constrict to increase the GFR?
the afferent arteriole sphincters
the efferent arteriole sphincters
Both afferent arteriole sphincters and efferent arteriole sphincters
Page 5
Reabsorbtion and Secretion
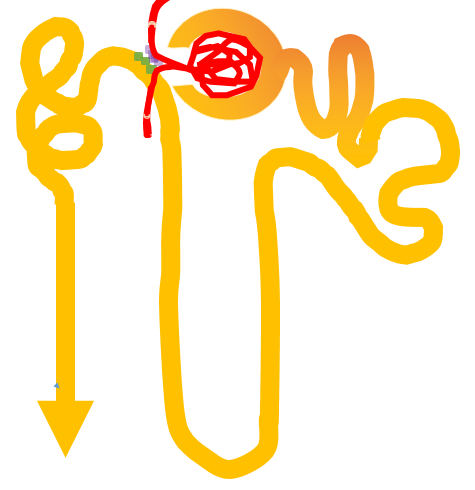
The ultrafiltrate has all kinds of good stuff in it, so you need lots of tubule cells to reabsorb the good stuff and secrete wastes. Nephron tubules are long, so that the urine passes a lot of cells before it goes out. To fit these long tubules in a small space, they are twisted and coiled.
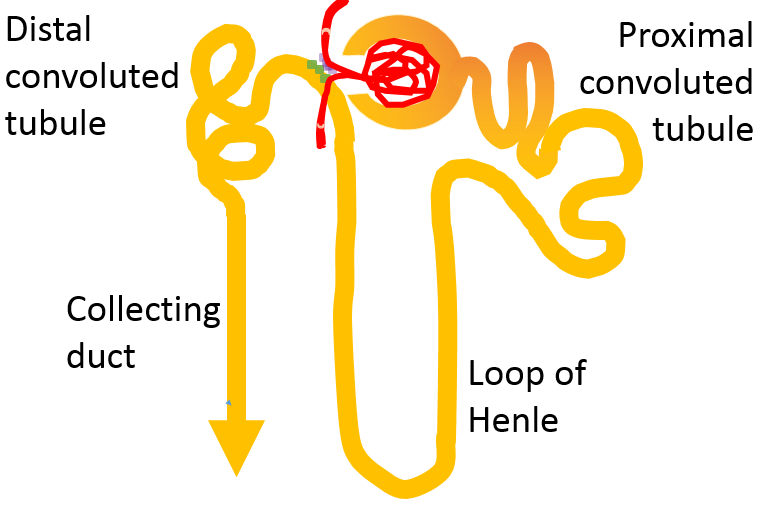
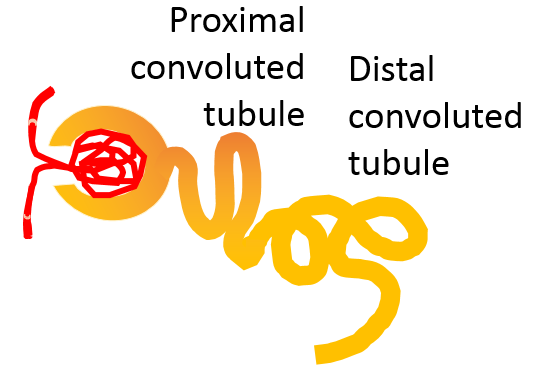
These twisted tubules are called convoluted tubules. The one closest to the glomerulus is the proximal convoluted tubule, and the one further away is the distal convoluted tubule.
Between the two convoluted tubules, the urine flows through a loop called the Loop of Henle. And at the end, it is collected in the collecting duct and sent out of the kidneys, on its way to the bladder.
The cells in each of these tubule segments have their own jobs.
Page 6
The Proximal Convoluted Tubule
The convoluted tubules do a lot of solute and water reabsorbtion - they pass solutes and water back to the blood. Proximal convoluted tubules are responsible for reabsorbing the majority of the solutes and water.1 They reabsorb most of the food molecules (like glucose or amino acids) and over half of the ions (like Na+, Cl-, and K+) Water follows all these back into the blood by osmosis, so the volume of ultrafiltrate has decreased by about 2/3 by the time it passes the proximal convoluted tubule. 2
1Curthoys, N. P., & Moe, O. W. (2014). Proximal Tubule Function and Response to Acidosis. Clinical Journal of the American Society of Nephrology : CJASN, 9(9), 1627–1638. http://doi.org/10.2215/CJN.10391012.
2Manski, Dirk. “Kidney: Physiology of the Tubular Reabsorption – Www.Urology-Textbook.Com.” Www.Urology-Textbook.Com, August 21, 2017. http://www.urology-textbook.com/kidney-tubular-reabsorption.html
Page 7
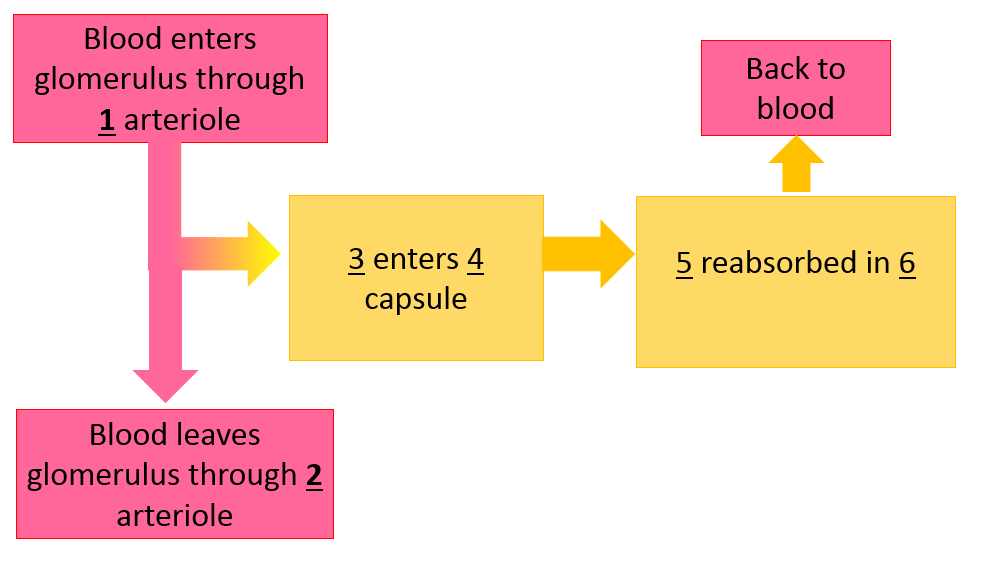
Item 1 should be:
the afferent arteriole
the efferent arteriole
The glomerulus
Item 2 should be:
the afferent arteriole
the efferent arteriole
The glomerulus
Item 3 should be:
urine
Food molecules and ions
Ultrafiltrate
Item 4 should be:
glomerulus
Bowman's capsule
Proximal convoluted tubule
Item 5 should be:
urine
Food molecules and ions
Food molecules, ions, and water
Item 6 should be:
Page 8
Distal Convoluted Tubule
The distal convoluted tubule, like the proximal one, can reabsorb Na+ and Cl-. It has some distinctive characters, though.
The place where the distal tubule ends and the collecting duct begins is sometimes called the connecting segment. In this area, the cells have a Na+/K+ ATPase pump that can actively reabsorb Na+ and actively secrete K+ into the urine. Each turn of the pump movs 3 Na+ into the blood and 2 K+ into the urine. Water will follow the majority of the ions by osmosis.
Which way will the water move between the urine and the blood?
it will be secreted from the blood to the urine
it will be reabsorbed back into the blood
Trick question, there's not going to be any net movement of water because ions are moving both ways.
When should the kidneys run this pump?
when blood pressure is high
when blood K+ is too high
When blood pressure is low
Page 9
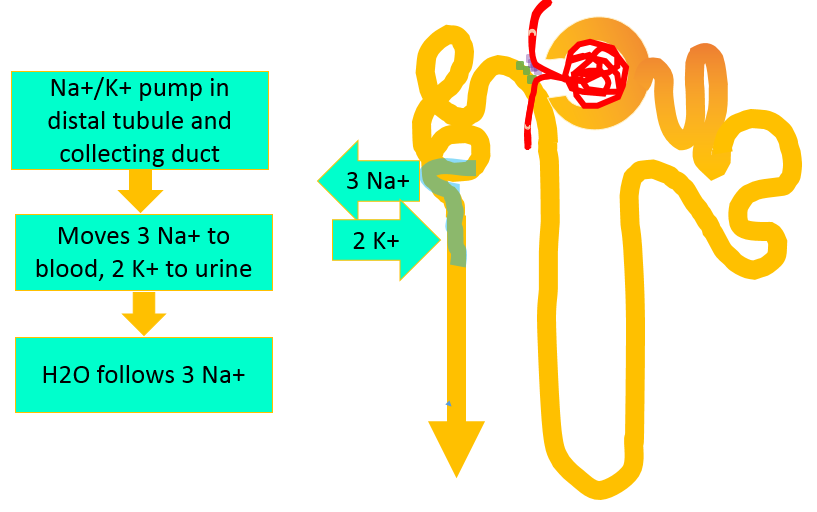
The distal convoluted tubules are important for balancing K+ levels in the blood, because they are able to secrete K+ into the urine with their Na+/K+ ATPase pumps. They are also important for maintaining blood pressure, because they move Na+ into the blood and water follows by osmosis. But what will tell them when to do this?
If you know the renin-angiotensin-aldosterone pathway, you know what hormone turns on the Na+/K+ ATPase; ALDOSTERONE.
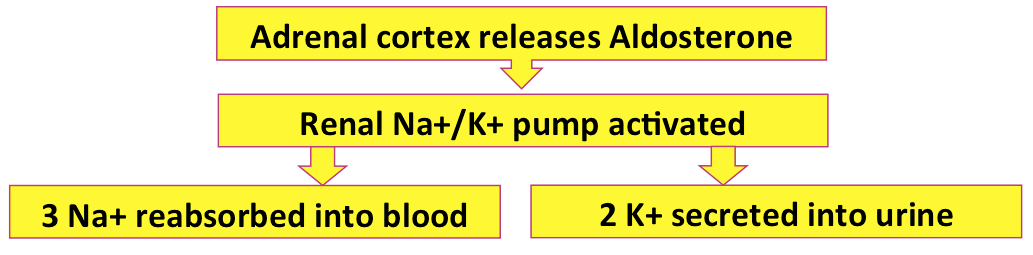
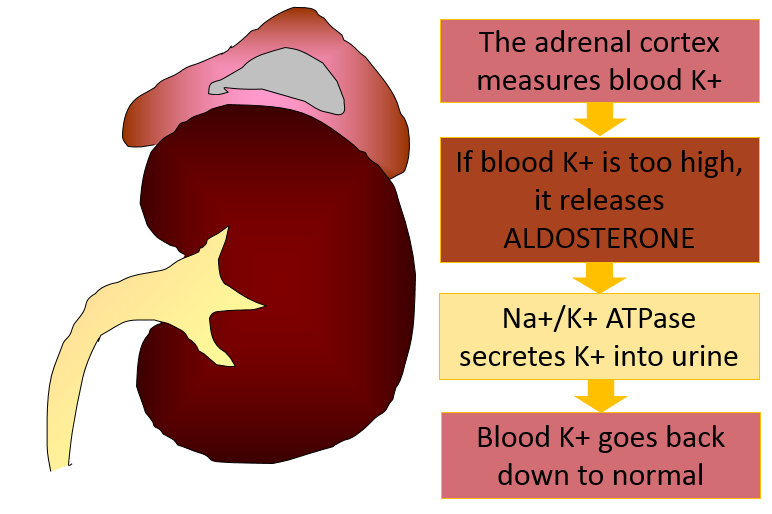
The first reason is very simple. The adrenal cortex, which makes the aldosterone, can measure blood K+. When the K+ concentration is too high, the adrenal cortex secretes more aldosterone, causing the distal tubule to secrete the excess K+ into the urine.
Page 10
The adrenal cortex is responsible for releasing aldosterone when blood K+ is too high. But we also want to release aldosterone when the blood volume has decreased. This is the job of the renin-angiotensin-aldosterone pathway.
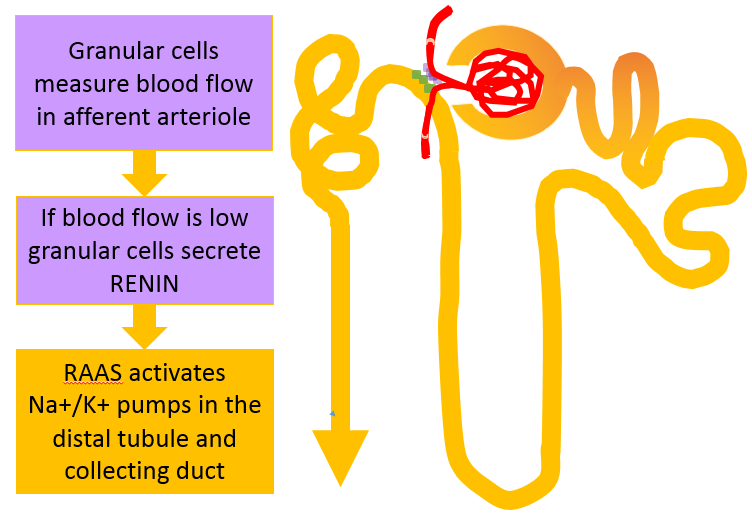
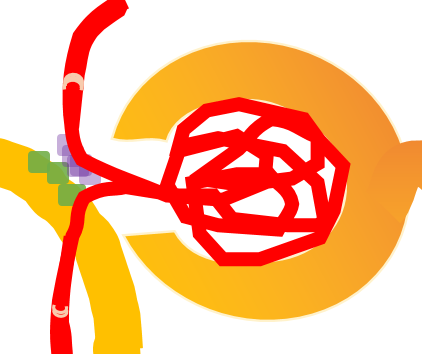
A specialized group of cells is found at the place where the glomerulus and the junction between the loop of Henle and the distal convoluted tubule are close together. This group of cells is called the juxtaglomerular apparatus (that just means 'close to the glomerulus').
One group of cells, shown in purple, is called the granular cells. These cells are attached to the afferent arteriole, and can detect how much blood is coming into the glomerulus. When blood flow decreases, they are responsible for releasing renin and starting the pathway which will eventually turn on the Na+/K+ ATPase pumps in the distal tubule and reabsorb Na+ and water to the blood.
That will raise blood volume, and bring the flow in the afferent arterioles back to normal.
How will the Na+/K+ ATPase pump affect the blood composition?
It will increase blood osmolarity and decrease blood K+
it will raise blood K+ but not change blood osmolarity
it will reduce blood K+ but not affect blood osmolarity. Blood volume will increase, though!
Page 11
The cells shown in green are the macula densa, a set of cells that are part of the tubule. They can measure how much urine is passing through, how much NaCl is in that urine, and some other compounds in the urine.
When there is too much blood being filtered, a lot of ultrafiltrate and NaCl will reach the distal tubule. The macula densa cells will release compounds that constrict the afferent arteriole and reduce the amount of filtrate being produced; also, the macula densa will decrease renin secretion, so Na+ and water are not reabsorbed into the blood. The combination of (1) constricting the afferent arteriole and (2) decreasing the blood volume by letting Na+ and water be lost in the urine will bring filtration back within normal levels.
If the kidney's filtration were too low, on the other hand, less filtrate and less NaCl would pass the macula densa. It would signal the afferent arteriole to dilate and increase renin release until filtration returned to normal levels.
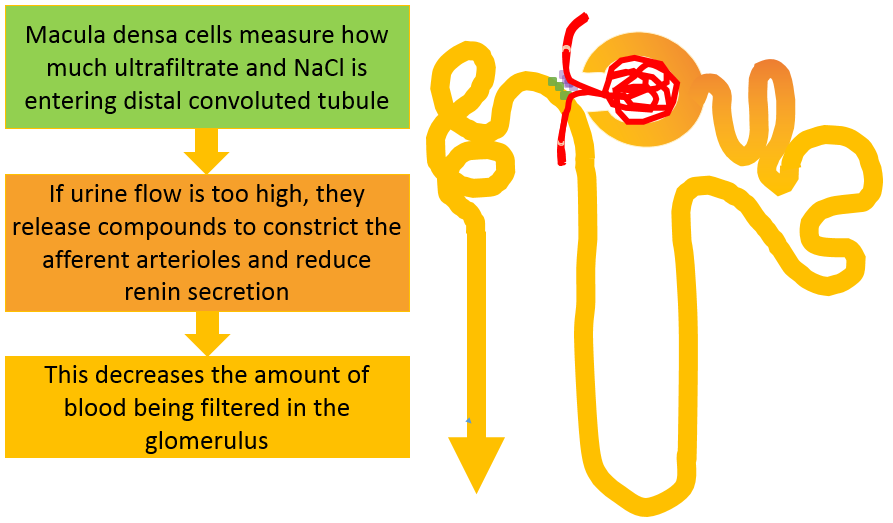
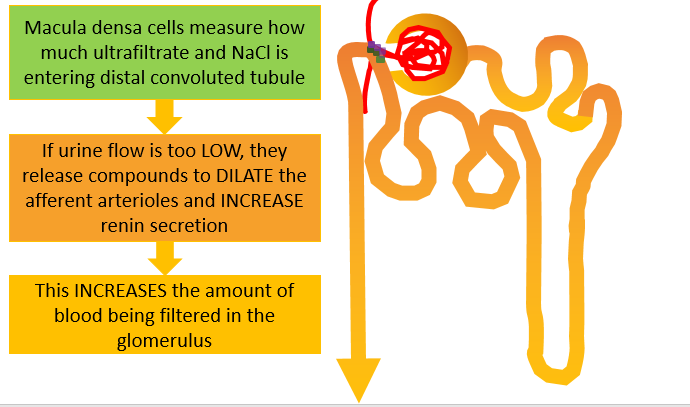
So to put it simply: the granular cells will adjust the reabsorbtion of Na+ and water to keep blood pressure stable, and the macula densa cells will adjust filtration and reabsorbtion of Na+ and water to keep urine flow in the nephron within normal limits. In this way, the kidney can keep on doing its job at a proper speed, even when your blood volume goes up and down.
Page 12
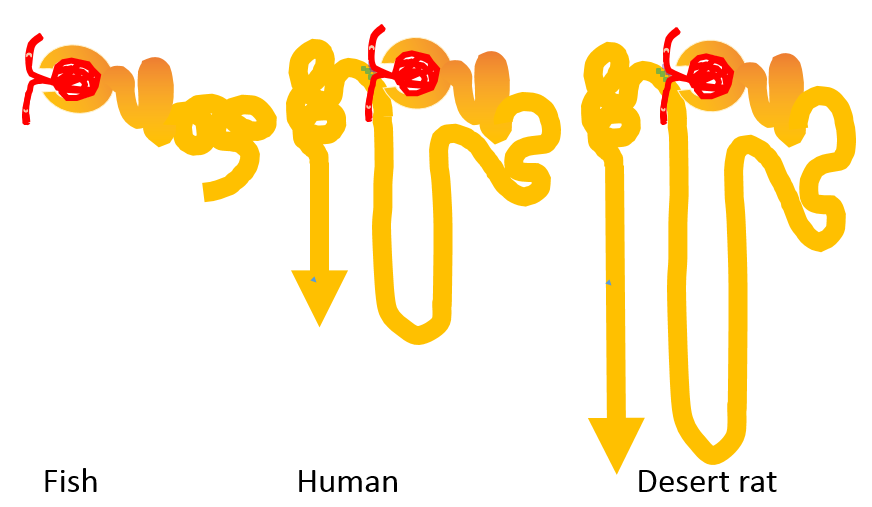
When you were an early fetus, this was all your nephrons had -- the glomerulus, Bowman's capsule, proximal convouted tubule and distal convoluted tubule. It's all fishes have, too. No Loop of Henle, no collecting duct. Why?
Here's a comparative diagram that may give you a clue. What are the Loop of Henle and the collecting duct needed for?
Page 13
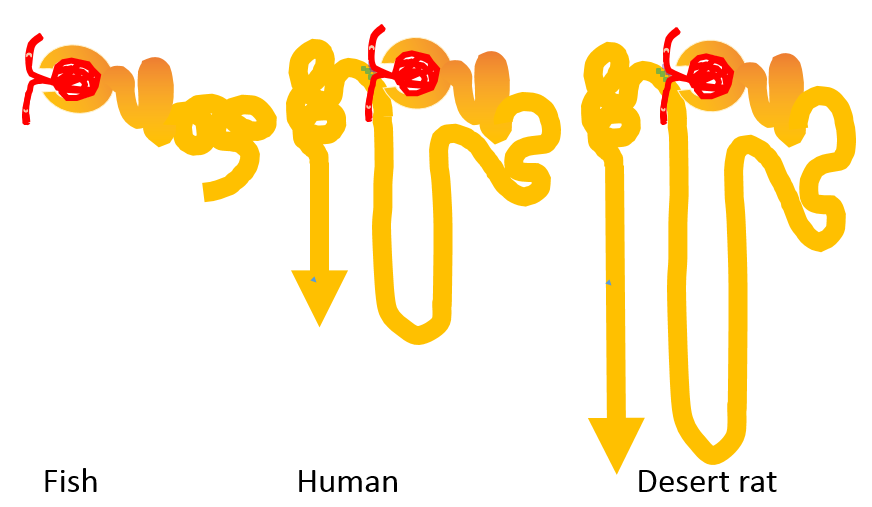
It's pretty obvious when you compare different animals - the Loop of Henle and Collecting Duct are for retaining water.
But how can they do it, when you don't have any such thing as a water pump in your body? The only way your body can move water is to move solutes, and then the water will follow the solutes; but then you have added both solutes and water to your blood, so the blood osmolarity has not changed.
That's not going to help a desert animal very much, because evaporation in the hot, dry desert will remove water from the animal's body. How can this animal retain just water, to keep its blood from getting dehydrated?
Let's look at the very clever way the Loop of Henle, collecting duct, and blood vessels work together to accomplish this.
Page 14
To begin with, we need to look back at the gross anatomy of the kidney. Here it is cut open to show the important layers, with one nephron shown in yellow so you can see how it is positioned.
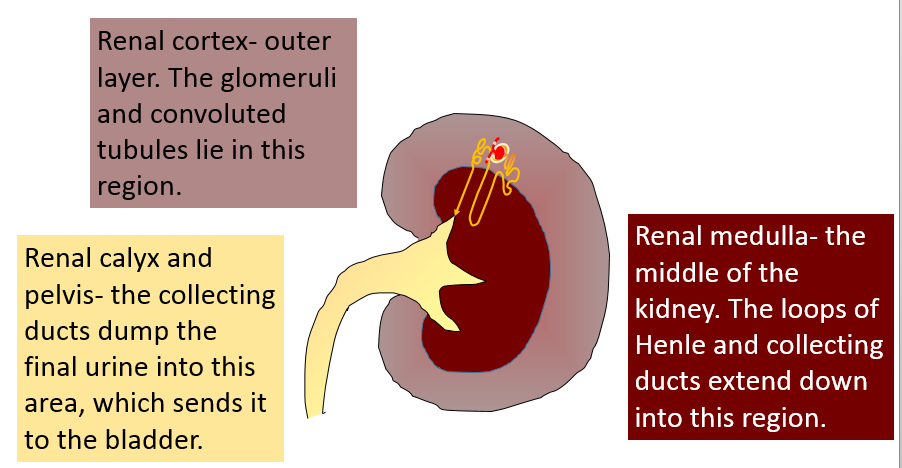
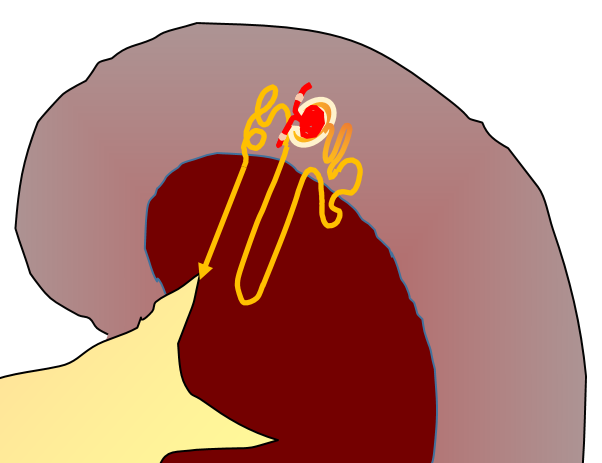
You can see that the loop of Henle and collecting duct run down into the medulla. This must be where they work their magic to return water from the urine to the blood! So let's look at how the medulla is different from the rest of the kidney.
Page 15
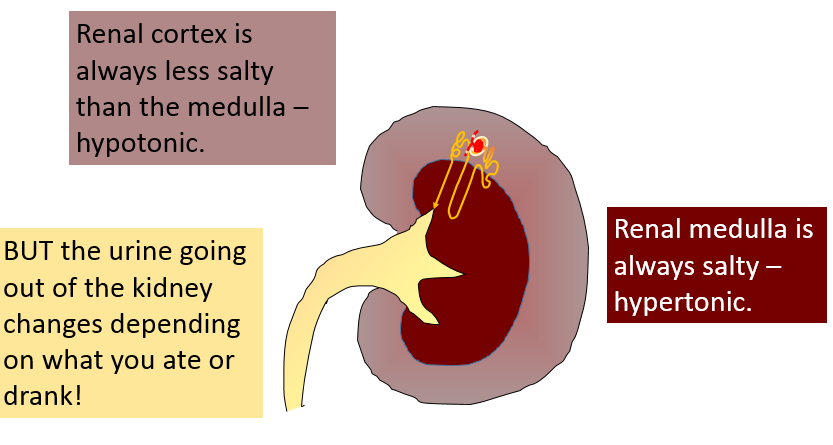
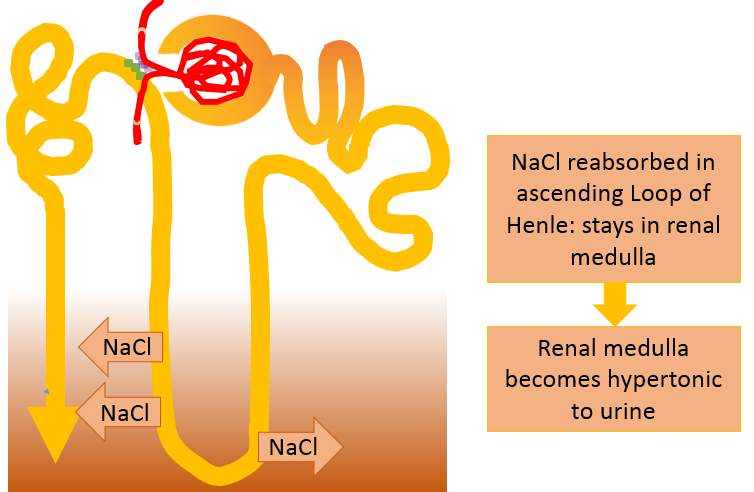
The medulla has one characteristic that makes it stand out - it is always really salty. It is hypertonic to the urine in the loop of Henle and the collecting duct.
How did the medulla get that salty? Turns out that the Loop of Henle did it! The loop has ion pumps that move salt out into the medulla.
Now that you know about the salty medulla, I bet you can predict what will happen as the urine flows down the collecting duct, through this hypertonic area. What do you expect?
water will move from the urine into the hypertonic medulla
there will be no net water movement, because the urine is flowing down to the calyx
water will move from the medulla into the urine
Page 16
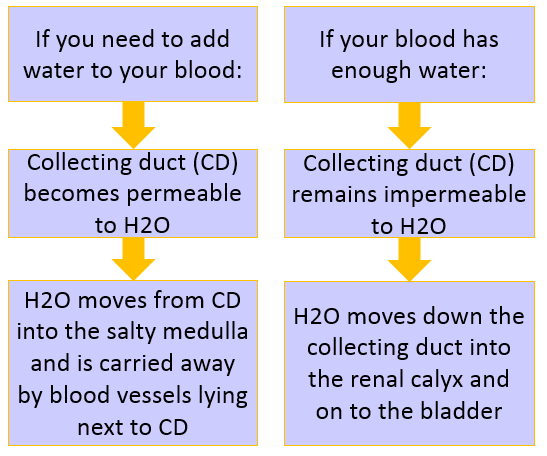
You figured it out! Water from the urine in the collecting duct will be reabsorbed into the salty medulla by osmosis. It will enter blood vessels carrying blood out of the medulla, and be carried away - returning vital water to the blood!
But this won't happen all the time. If you drank a lot of water, you wouldn't need to retain it - and in fact, you wouldn't. We've all experienced really dilute, watery urine after we drink a lot of water. So your collecting duct must be able to turn water reabsorbtion on or off.
In fact, that's exactly what your collecting duct does. When you need to reabsorb water into your blood, the collecting duct lets water pass through its walls, from the urine back into the medulla and the bloodstream. When you have plenty of water and need to dump some of it out in your urine, the collecting duct's walls become waterproof, and all the water inside runs straight to the renal calyx and the bladder.
When do you think the collecting duct will become most permeable to water?
when the blood is hypotonic to the cells
when the blood volume is too low
when blood K+ is too high
when the blood is hypertonic to the cells
Page 17
The collecting duct doesn't decide whether to let water through on its own. Like the distal tubule, its activity is controlled by a hormone.
Anti-diuretic hormone (ADH)
The name means 'against urination.' If you have a lot of ADH, you won't produce very much urine. So what is ADH doing to the collecting duct?
making it impermeable to water
making it more permeable to water
nothing; the connecting duct doesn't control urine volume
Page 18
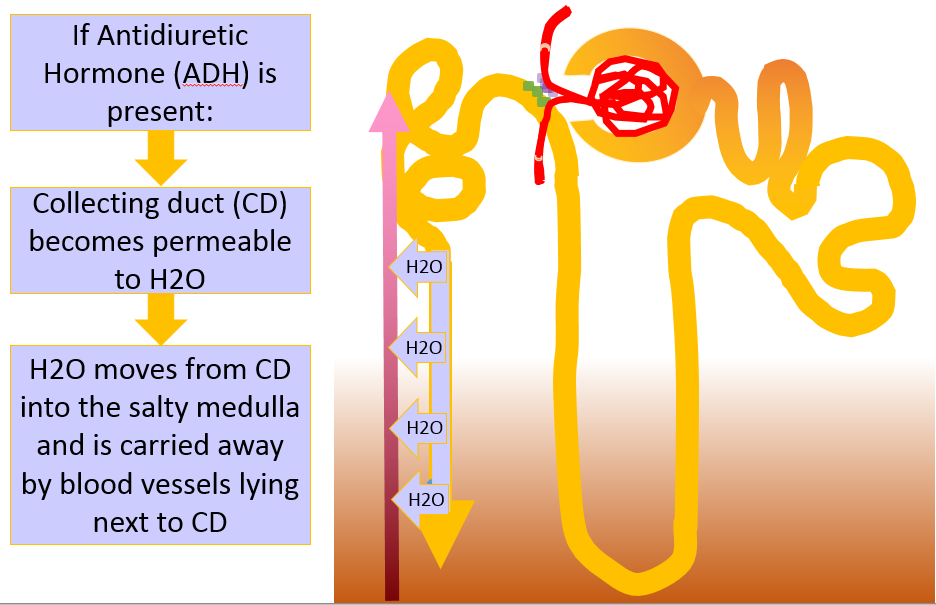
Your posterior pituitary releases ADH into the blood when the blood pressure is low or the cells start to shrink from dehydration. This is the most effective way you have to move water from your urine back into your blood.
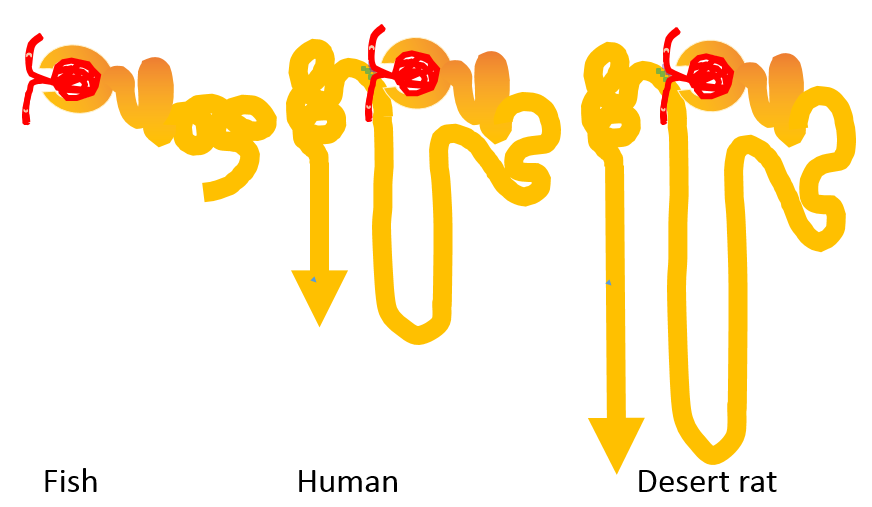
So looking back at these comparative kidneys, it seems pretty clear why they look the way they do! Animals who live in water and never need to worry about dehydration don't need the collecting duct at all. But animals who live in dry environments need a long collecting duct, so they will have the most duct surface to reabsorb water into the blood.
Page 19
You've come to the end of the kidney review.
Think you have the basics down? See if you can choose the right terms in this summary.
Blood enters each nephron through the efferent arteriole / afferent arteriole, which brings it to a capillary bed called the glomerulus / Bowman's capsule. The blood is filtered at this structure and everything except cells, lipids and proteins / K+ and water crosses over into the Loop of Henle / Bowman's capsule. The fluid in the nephron is called urine / ultrafiltrate.
Lots of the solutes and water are reabsorbed into the blood right away by cells of the proximal convoluted tubule / distal convoluted tubule. Then the fluid passes into the distal convoluted tubule / Loop of Henle. This structure dives down into the renal medulla, where urine is secreted from the medulla / NaCl is reabsorbed into the medulla.
Because of this, the medulla of the kidney is hypotonic to the urine / is hypertonic to the urine. This will be important later, if the collecting duct / glomerulus needs to reabsorb some water into the blood.
Meanwhile, the fluid moves on into the distal convoluted tubule / proximal convoluted tubule. This is where the water pores / Na+/K+ ATPase pumps are located.
These pumps turn on when they are exposed to aldosterone / ADH. When they run, they'll move 3 Na+ out of the blood / into the blood and 2 K+ into the blood / out of the blood into the urine. Water will move out of the blood / into the blood
How does the body know when to run the pump? When the blood K+ is low / high, the adrenal cortex will release aldosterone. When the blood flow in the afferent arteriole is high / low, the granular / smooth cells in the proximal tubule / juxtaglomerular apparatus will release renin, which will start the renin-angiotensin-aldosterone system and also increase aldosterone levels.
Aldosterone will increase / decrease blood K+, increase / decrease blood volume, and increase / decrease / not change blood tonicity.
Suppose your blood were dehydrated, though? You would need to reabsorb water from the urine, and the urine is almost out of your kidney. It only has one segment of the tubule to go through - the collecting duct. This is your last chance to reclaim some of that water before it's sent to your bladder and out.
Good thing the collecting duct goes down through the cortex / medulla - and that area is hypertonic / hypotonic to the contents of the collecting duct. So water will diffuse out of the medulla into the collecting duct / out of the collecting duct into the medulla That water will be carried away by blood vessels, making the blood more hypotonic / hypertonic.
You don't always need to save water, though - only when you're dehydrated. So your collecting duct doesn't always let water cross its walls. The only time it will let water do that is when the hormone ADH / aldosterone is present.
Good work! Now you should be able to apply it to some cases. Try to explain each situation yourself first, and then click on the question to see the correct answer.
This is the end of the kidney tutorial. Happy studying!