This tutorial will take you through the sequence of events in the adaptive immune response.
You can navigate through this tutorial using the buttons at the top of the screen.
The tutorial will ask you questions. Click on your chosen answer to see feedback; click the answer again to make the feedback disappear. When you're finished with one page, click the navigation button for the next page to move ahead.
Have fun! Click on button '1' to see the first page of the tutorial.
Page 1
If your body's been injured, it has already deployed the inflammatory response to address the problem. Remember that the inflammatory response, or 'innate immune response,' is pretty much always the same - it uses the inflammatory mediators made by injured cells and the white blood cells already circulating in the blood to defend against any kind of injury, from an infection to a stubbed toe.
The inflammatory response includes cells like neutrophils and macrophages that can devour bacteria and other pathogens - and it includes chemicals like C-reactive protein that can also attack pathogens, and responses like the formation of exudate that can trap them and keep them from moving around. But nothing works all the time, and sometimes the pathogens multiply too fast for these responses to keep them under control.
That's when your Adaptive Immune Response becomes important.
Page 2
Adaptive means something that can change to match its circumstances. That's what the Adaptive Immune response does - it changes. The adaptive immune response to measles is different than the response to influenza. These responses target specific pathogens, with white blood cells that look for the pathogens and kill them and specifically designed antibodies that can bind to the pathogens and kill them.Let's introduce the players in this system: the B and T lymphocytes.

graphics from Microsoft Clip Art.
B lymphocytes
The B-lymphocytes are white blood cells, so like all other white blood cells they are created in the bone marrow. They have some pretty amazing abilities, though: they're antibody builders. Antibodies are special proteins designed to latch on to a specific pathogen.Another special thing about B lymphocytes is that they are all a little different from one another. They're individuals.
graphics from Microsoft Clip Art.
T lymphocytes
Here are the T lymphocytes. They were also made in the bone marrow, and they also are all individuals. But you can see that they're not ready to go to work yet. They don't really know what they ought to be doing! These cells will need more training, and they'll go to the thymus to get it. That's why they are called T cells.But before we follow these cells any further, let's clear something up. What do I mean when I say they're different from one another? After all, inside your body they are not different colors.
What I'm referring to is the shapes of proteins on the cell surfaces. The different T and B cells have differently shaped receptor proteins on their surfaces, which means they will bind to different things. This is very important for you, because it means that no matter what kind of pathogen infects you, you probably have a B cell and a T cell that can bind to it.
NEW TERM ALERT!
When T or B cells bind to pathogens, they are attaching to the pathogens' cell surface molecules. The molecules that can bind to receptors on the B and T cells are called antigens. 'Anti' means 'against', and 'gen' means 'causing' - so these are molecules that cause the immune system to react against them.
Every cell has molecules all over its surface, so potentially your immune system could attack any cell - if B and T cells had receptors for its cell surface antigens.
Page 3

graphics from Microsoft Clip Art.
So what is this lymph I speak of?
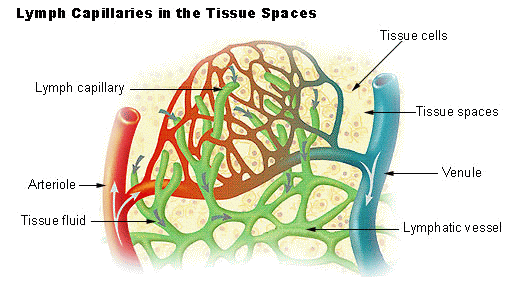
Lymph capillaries by U.S. National Cancer Institute's SEER Program, Public Domain.
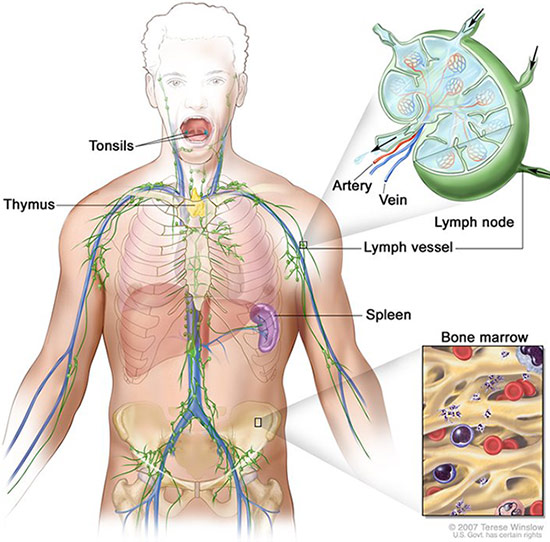
Lymphatic System by U.S. National Cancer Institute's SEER Program, Public Domain.
Page 4
Meanwhile, what have your T lymphocytes been up to in the thymus?The thymus trains the T cells to be managers. They learn how to tell when the immune system should turn on, and how to tell foreign cell surface proteins from your own cell surface proteins, so your immune system will not attack your own cells. I think you would agree that this is a pretty important job!
There are basically two classes in thymus college, and both of them are taught by specialized cells in the thymus.
graphics from Microsoft Clip Art.
The first class is in attaching to MHC proteins.
Why is this so important? It's because of the T cells' role in deciding which antigens should be attacked. A T cell can't just start attacking on its own; it should only attack antigens from real infectious organisms, the kind that have caused an inflammatory response. The kind that antigen presenting cells are eating, or infected cells are making.
Cells that have eaten pathogens, or infected cells that are being forced to make pathogens, will take some of those pathogens' cell surface antigens and present them, attached to special proteins on the cell surface. These are called MHC proteins.
The first class in the thymus, then, is to sort out the T cells that will attach to MHC proteins from the ones that won't. T cells that ignore the MHC proteins will not progress any further.
Page 5
graphics from Microsoft Clip Art.
graphics from Microsoft Clip Art.
Page 6
graphics from Microsoft Clip Art.
O-O
And it looked like such a friendly professor!
O-O
Yep, that's life in thymus college. If you fail a test, the professor kills you.But there's really no way around it.
Remember, all those little T cells have different cell surface receptors, so they can attach to different antigens. If one of them has a cell surface receptor that attaches to your self-antigens, it could cause a nightmare - it would attack your own tissues and destroy them. So the thymus cells have to make sure none of the self-reactive T cells get out of the thymus.
They don't always succeed; that's one reason people get autoimmune diseases like type I diabetes, or systemic lupus (another reason is that self-antigens can be similar to antigens from actual diseases, and then the T cells attacking those diseases can make mistake and attack the self-antigens instead).
Page 7
free image from Clipartbest.com
Here come the mature T cells, out of the thymus and straight into the lymphatic system, to join the B cells.
They're all ready to start attacking infections - when the antigen presenting cells tell them to. Until that happens, we call them naive T cells.

graphics from Microsoft Clip Art.
The T helper cells will be the ones that boss the other lymphocytes around, telling them whether they ought to attack an antigen or not. These are the cells that will interact with the antigen presenting cells. They'll attach to MHC proteins on those cells to see what antigens are causing a problem in the body.
The T cytotoxic cells are the 'muscle.' After T helper cells tell them what to do, they will go out in the body searching for abnormal cells … but we'll see how that works a little later.
Nowadays, we measure these cells by looking for the special proteins on their surfaces. That's why we call the Th cells CD4+ and the Tc cells CD8+ - because CD4 and CD8 are proteins on their surfaces. You might see these values on patient's charts, especially if they have problems with their immune system. If the CD4+ count goes down, the patient's immune system won't work properly.
Page 8
That was a lot of information! It's time to do a little review. Choose the correct answers in this summary of what you've learned so far.
The adaptive immune response depends on white blood cells called basophils / lymphocytes. These cells are found in large numbers inside the lymph, which is fluid removed from your tissues by lymph capillaries / fluid delivered to your tissues by lymph capillaries. This fluid is filtered in lymph nodes / the kidneys before it is returned to the blood, so those are the perfect place for the body to detect and react to infections.
The lymphocytes were created in the liver / bone marrow.
One group of them - the B cells / T cells - go straight out into the lymph and blood to patrol for pathogens. They can identify pathogens if their receptors can attach to the pathogens' cell surface antigens / flagella. Each lymphocyte has unique receptor molecules, so it can attach to different pathogens. That's what allows your immune system to protect you from so many different diseases.
The second group of lymphocytes, the T cells / monocytes, go to the spleen / thymus. There, they learn two things: first, to interact with cells by attaching to their self-antigens / MHC proteins and looking there for the pathogens they ought to attack. The second lesson they learn is to never attack a self-antigen / neutrophil. Lymphocytes that attacked your own cells would be a really big problem!
Only lymphocytes that pass the two tests survive to get out in the blood.
They differentiate into two types, the monocytes and macrophages / T helper cells and T cytotoxic cells. T helper cells are also known as CD4+ / CD8+ and T cytotoxic cells are also known as T killer cells or CD8+ / dendritic cells.
Now your body has a full set of mature lymphocytes. But they are still naive, meaning they haven't seen action yet! Let's see what happens when they actually have to respond to an emergency.
Page 9
The immune response is turned on after the inflammatory response, so let's begin by looking at the events in the cellular response of inflammation.
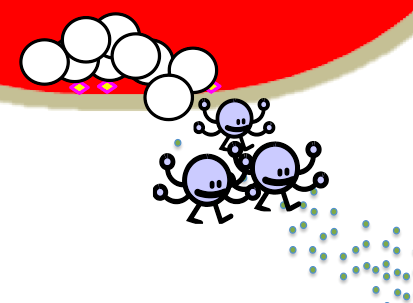
graphics from Microsoft Clip Art.
Remember when the monocytes crawled out of the blood into the injured tissues, following the trail of inflammatory mediators released by the injured cells and mast cells? They grew tentacles and turned into macrophages. Their cousins, dendritic cells, were already in the tissue.
These cells will get busy eating pathogens.
Other cells in the area aren't so lucky. If the pathogen is a virus, it will be invading some of your cells and turning them into virus factories.
graphics from Microsoft Clip Art.
Both macrophages and infected cells have a way to let the immune system know about those pathogens, however - their MHC proteins.
Page 10
You've heard of MHC proteins before, but let's take a closer look at them.
Major Histocompatibility Complex
They're called this because they are the proteins that control whether an organ for transplant is compatible with the recipient. If they don't match, the recipient's immune system will destroy the transplanted organ.All your cells have MHC proteins, but they come in two types.
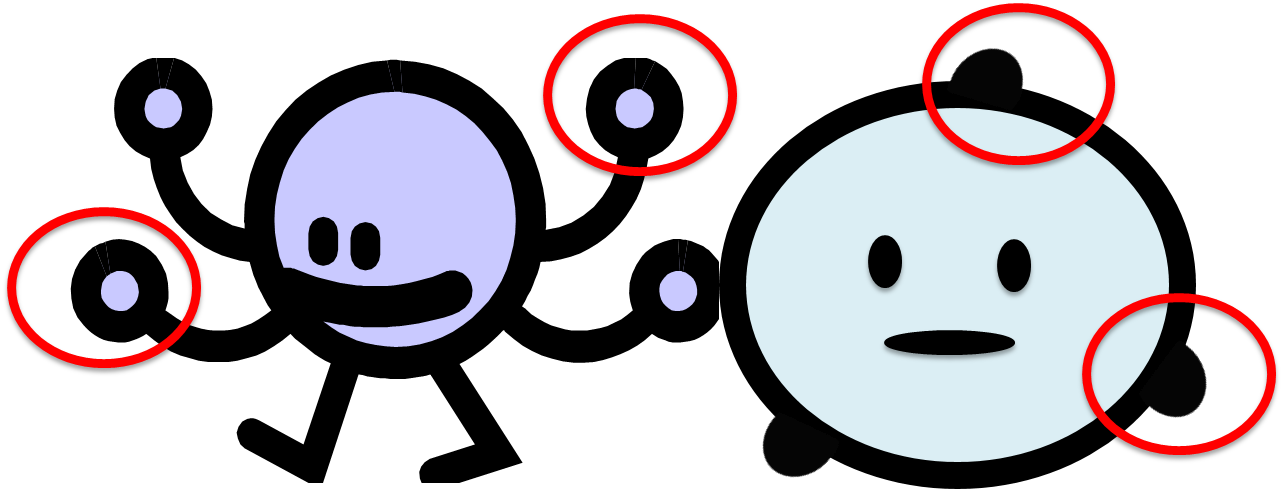
graphics from Microsoft Clip Art.
See them, with the red circles around them? You can see that the ones on the dendritic cell look different from the ones on the regular body cell. So we call the ones on the macrophages and dendritic cells MHC II, and we call the ones on regular cells MHC I. They both do the same thing for the cell that has them: they serve as a place to put antigen molecules from pathogens, so the cell can alert the immune system to fight that pathogen.
Page 11
OK, back to the infected tissue! The macrophages and dendritic cells have been eating the pathogen, and some of your poor cells have been infected by it. That means that all of these cells have antigens from the pathogen inside them...
graphics from Microsoft Clip Art.
and the cells will put those antigens out on their MHC proteins, for the T cells to see.
graphics from Microsoft Clip Art.
There's just one problem - do you see any T cells anywhere around? No, they're in the blood and the lymphatic system, wandering from lymph node to lymph node.
Page 12
Antigen-Presenting Cells
Here's where the dendritic cells earn their keep -- they will carry the antigen all the way from the tissue into the lymph capillaries, all the way up to the nearest lymph node.
graphics from Microsoft Clip Art.
Here's the thing, though: a T helper cell will only react if it has cell surface receptors that match the antigen the antigen-presenting cell is presenting. Remember that all the T cells are different from each other, and have different receptors?
So what if there isn't any T cell in that lymph node with a receptor to match the antigen an antigen-presenting cell is presenting? The antigen-presenting cell will wait around in the lymph node. T cells are moving around from node to node, and whenever they enter a lymph node they 'browse' through the antigen-presenting cells waiting there, to see if there's anything they match. Eventually, a T helper cell that matches the antigen will find this dendritic cell, attach to it, and become activated.
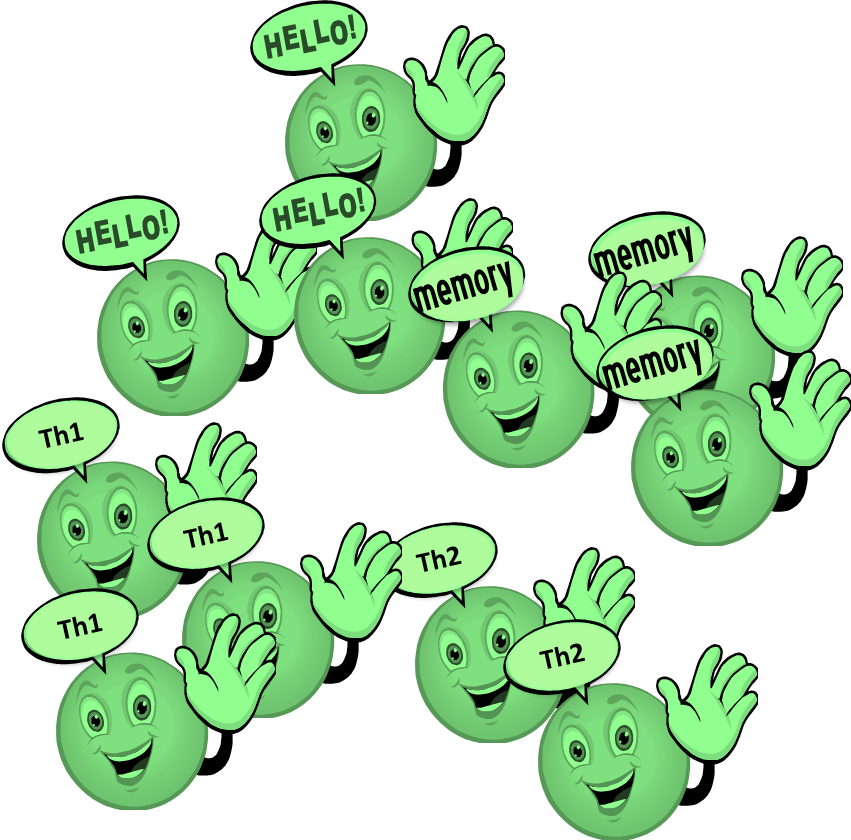
graphics from Microsoft Clip Art.
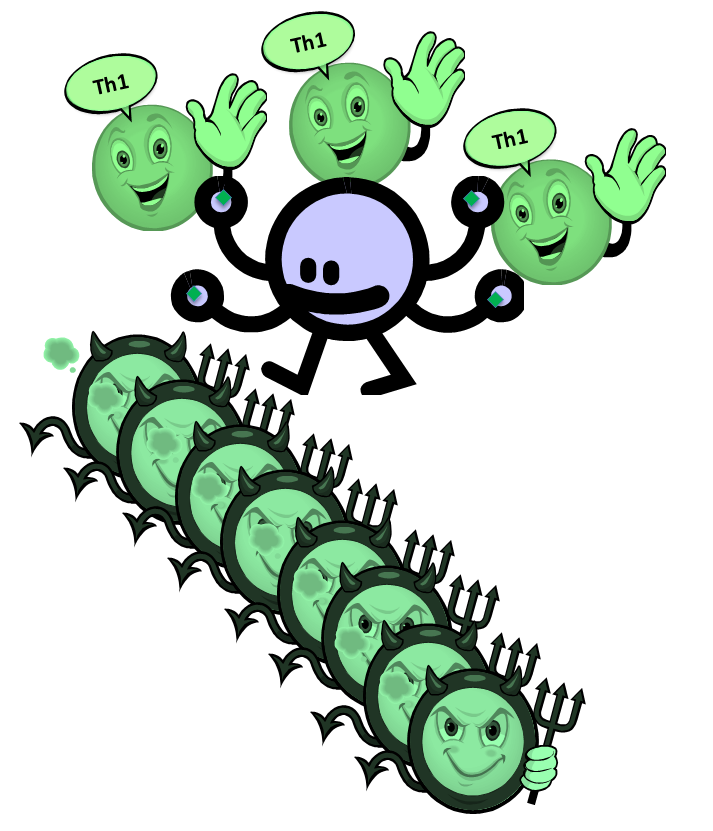
1. T-helper 1 cells will tell the T cytotoxic cells what to do.
2. T-helper 2 cells will tell the B cells what to do.
3. T helper memory cells will hang around waiting. If this antigen ever appears again, they will remember that it was OK to attack it.
4. T suppressor cells, or Regulatory T cells, will help turn down the immune response when it isn't needed any more.
Page 13
graphics from Microsoft Clip Art.
Pretty soon, a T cytotoxic cell comes browsing along, looking at what the antigen-presenting cells have put on their MHC I proteins. If it can attach to this antigen, the antigen-presenting cells and the T-helper 1 cells activate it, and that T cytotoxic cell begins to divide.
graphics from Microsoft Clip Art.
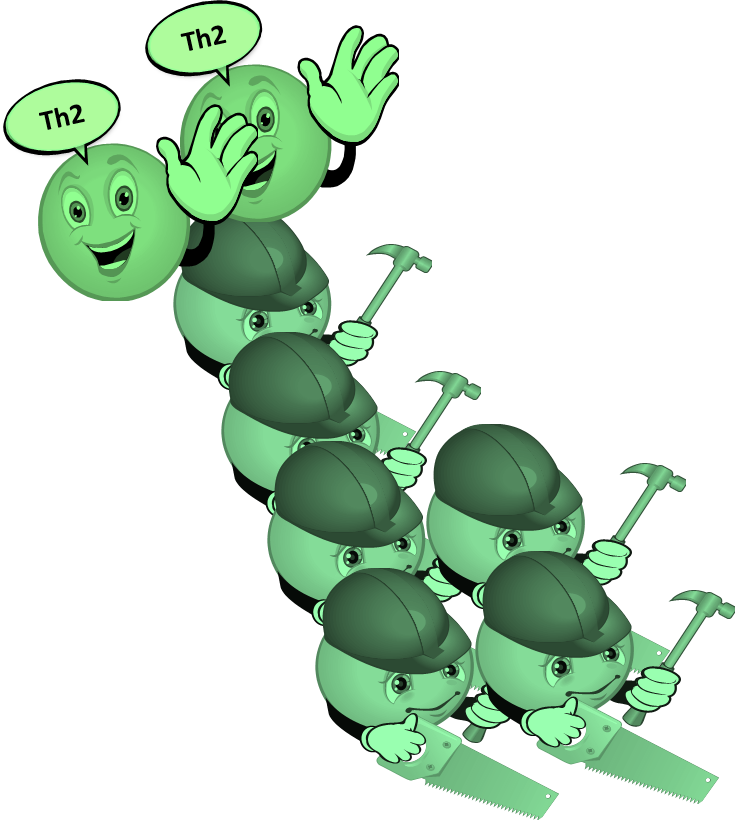
At the same time, the T-helper 2 cells are activating B cells that can bind to this antigen, and they too begin to divide.
Your lymph node is filling up with cells! That's why you get swollen lymph nodes near an infected area.
What would happen to you if you didn't have any antigen-presenting cells?
You wouldn't produce any naive T cells
Page 14
graphics from Microsoft Clip Art.
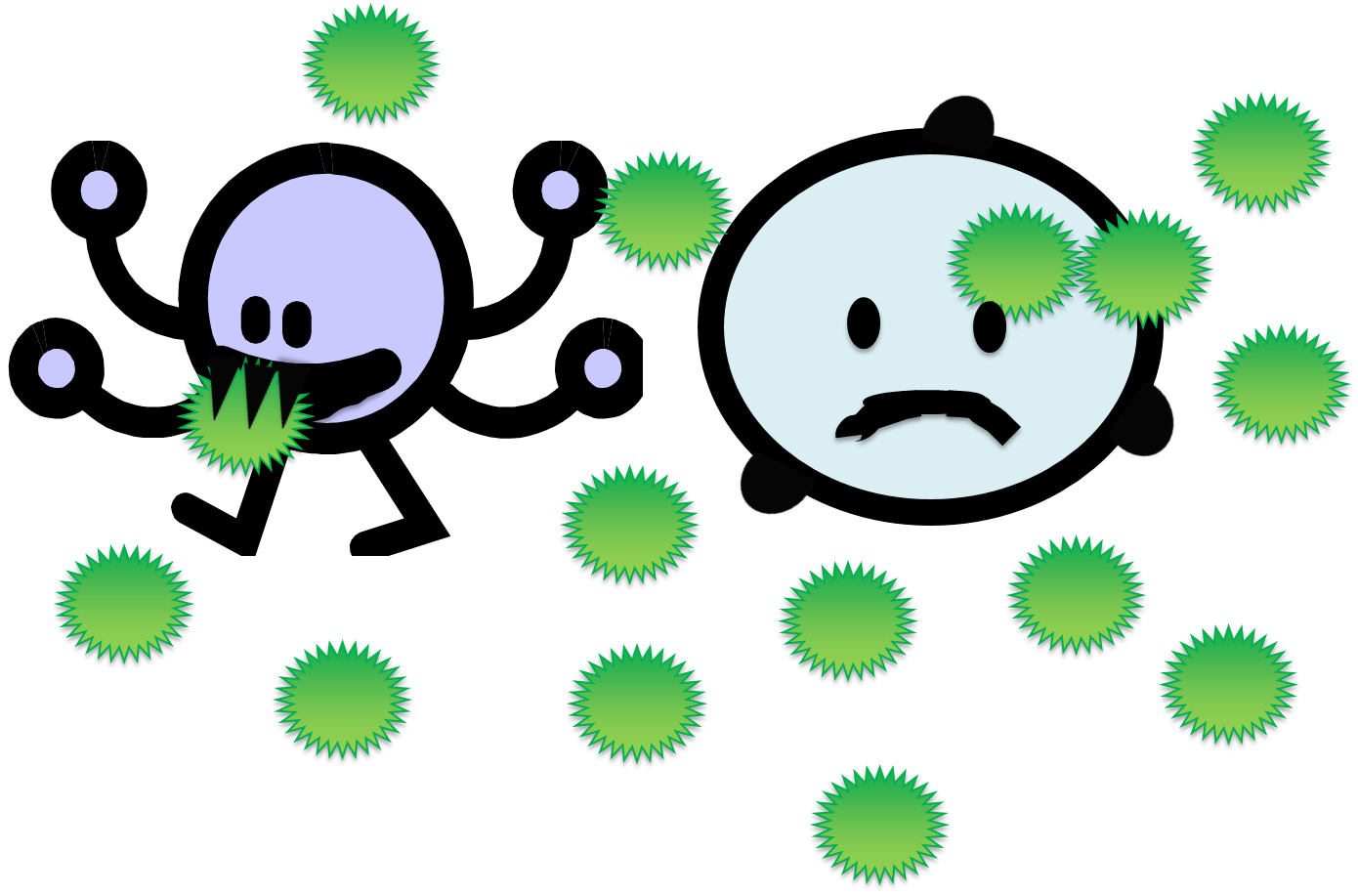
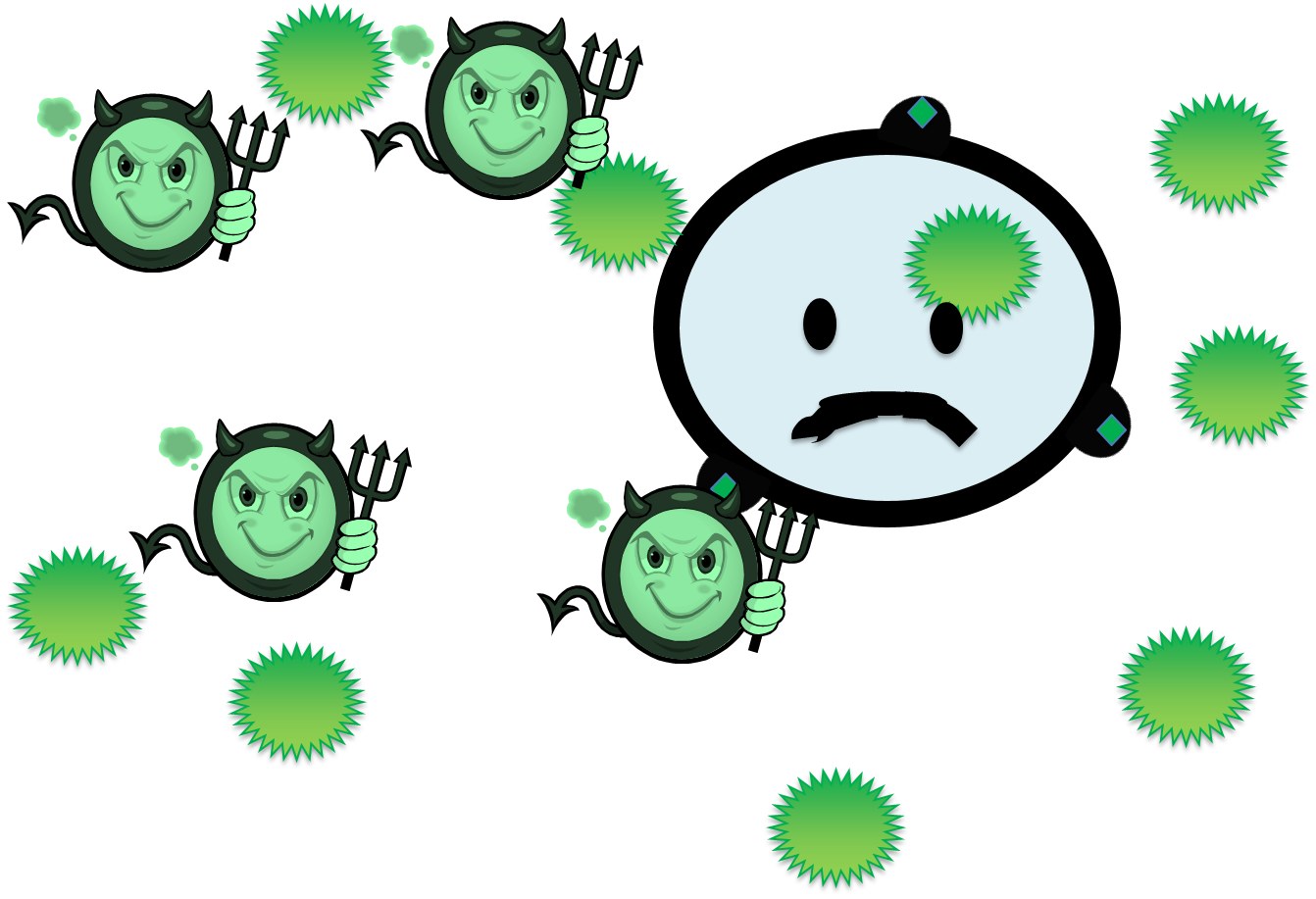
They go out into the blood, looking for the antigen - but the only place they look is on the MHC proteins of infected cells. Remember our poor infected cell?
Once a T cytotoxic cell finds the antigen it can bind with on the MHC protein of an infected cell, it binds to that cell and ...

graphics from Microsoft Clip Art.
This is called the cell-mediated immune response.
But the T cytotoxic cell didn't do a thing about all those other pathogens floating in the blood! Who's going to clean them up before they infect a whole bunch more body cells?
That would be a job for the B cells.
Page 15
graphics from Microsoft Clip Art.
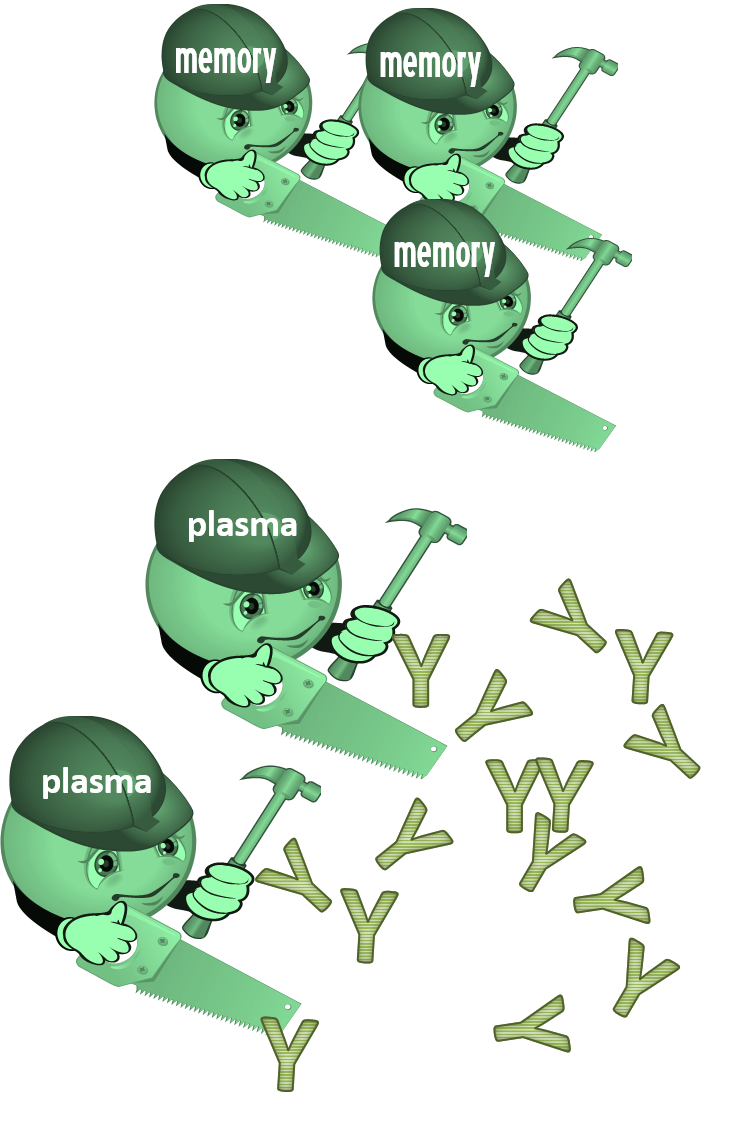
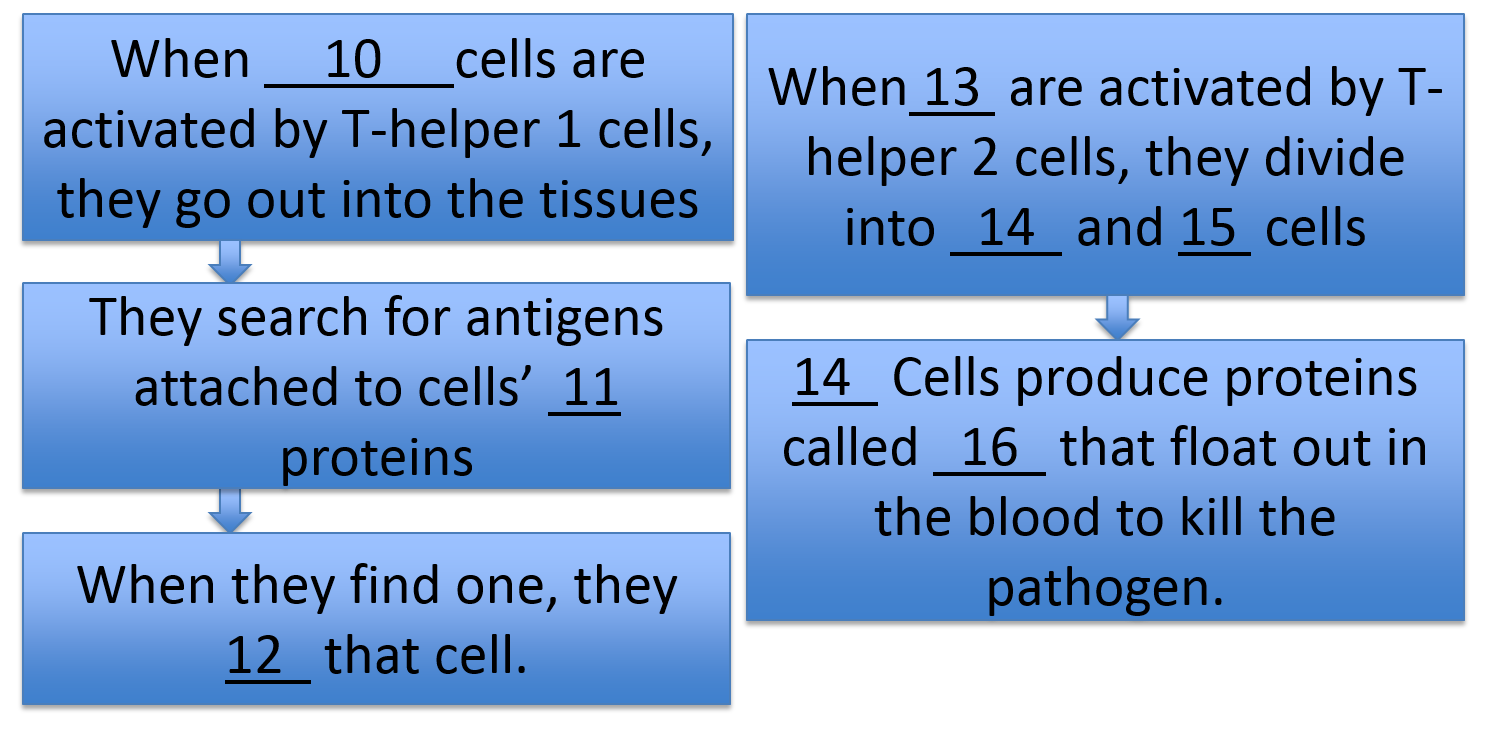
1. Plasma cells - these cells build proteins called antibodies or immunoglobulins. They are proteins designed to stick to the antigen. We draw them like Y's because that is what they're shaped like - they have a notch on each top branch of the'Y' that the antigen will fit right in to.
graphics from Microsoft Clip Art.
The antibodies float out in the blood and attach to the antigens. They can mark those antigens for destruction by white blood cells or toxic blood proteins, or they can make them stick together, or block their ability to infect your cells. And as long as you have enough antibodies floating in your blood, you will be protected against that pathogen - because as soon as it gets into the blood, an antibody will attach to it.This is called the humoral response.
2.Memory B cells - these will remember that the T-helper 2 cells said it was OK to attack this antigen. The next time you encounter the antigen, the B cells won't have to wait for permission before fighting it off.
Page 16
Review time! Choose the right term for each of the blanks in this flow chart.
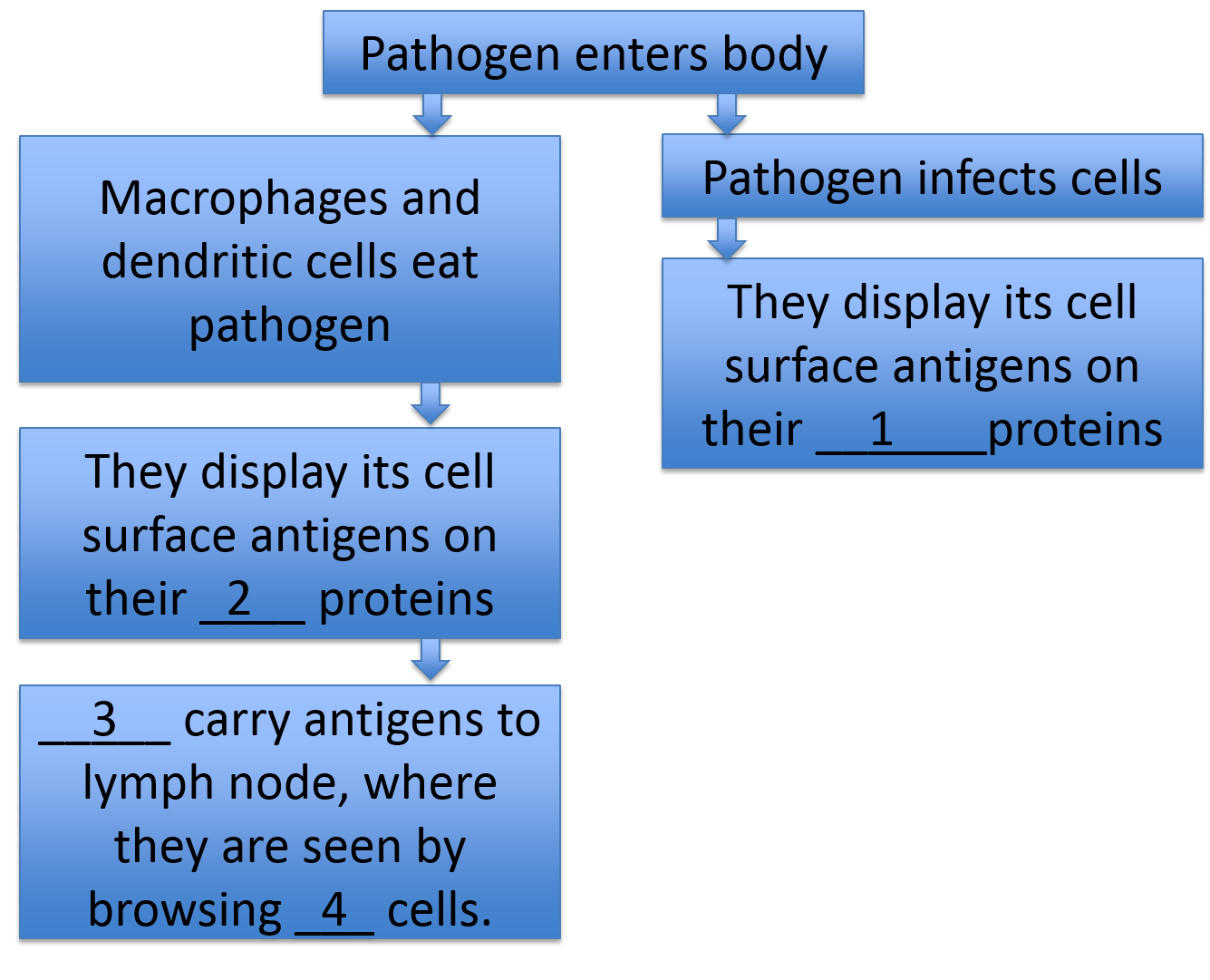
Item 1 is: MHC I / MHC II / antibody
Item 2 is: MHC I / MHC II / antibody
Item 3 is: macrophages / neutrophils / dendritic cells
Item 4 is: macrophages / B cells / T cells
Item 5 is: Macrophages / T helper / T killer
Item 6 is: MHC I / MHC II / antibody
Item 7 is: T-helper 1 / T-helper 2 / B
Item 8 is: T-helper 1 / T-helper 2 / T cells
Item 9 is: T-helper 1 / memory T-helper / memory B cells
Page 17
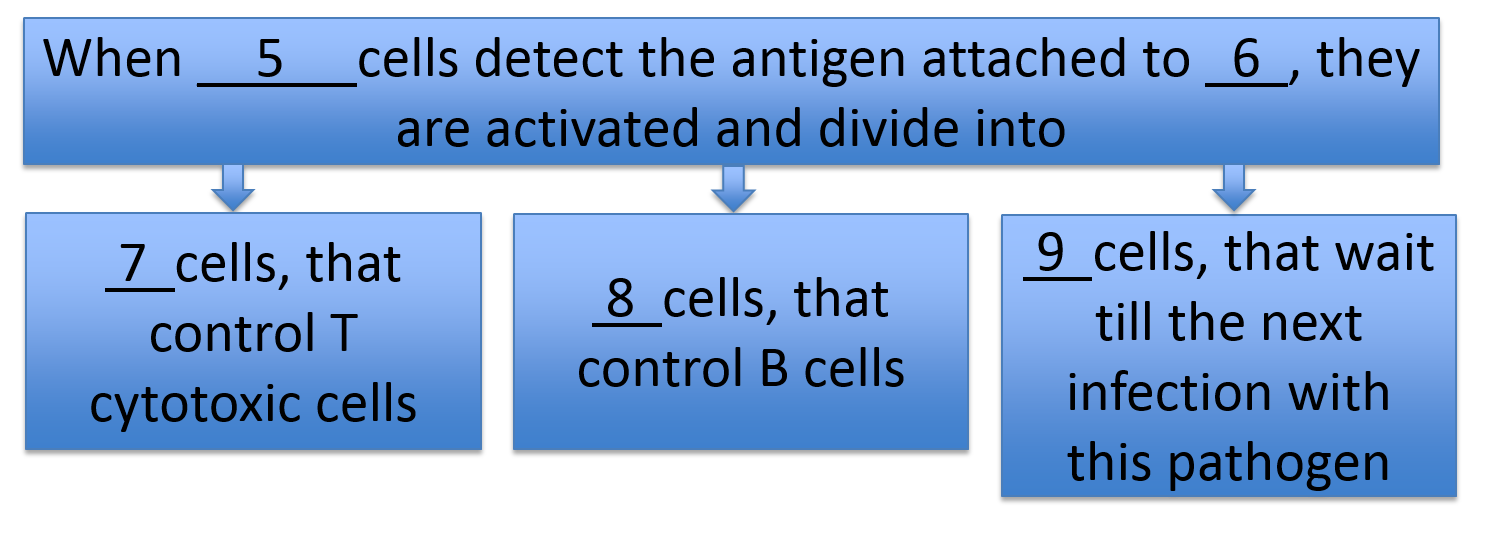
Item 10 is: MHC I / pathogen / T cytotoxic
Item 11 is: MHC I / MHC II / antibody
Item 12 is: heal / kill / move away from
Item 13 is: macrophages / B cells / T cells
Item 14 is: Macrophages / plasma / T killer
Item 15 is: MHC I / memory B cells / antibody
Item 16 is: T-helper 1 / antibodies / antigens
Good work! You've made it through the review of the immune system. Go relax!
Sources used in creating this tutorial include:
Porth, C., 2015. Essentials of Pathophysiology. 4th Edition. Lippincott, Philadelphia, Pa.
Kindt, T.J., R. A. Goldsby, and B. A. Osborne (2007) Kuby Immunology, 6th ed. W. H. Freeman.